Subclavian artery disease (stenosis or occlusion)—a disorder where the large artery beneath the collarbone (the subclavian artery) becomes narrowed or blocked, compromising blood flow to the arm and potentially affecting circulation to the brain. Blood supply is life. When arteries supplying key parts of the body become narrowed or blocked, the resulting ischemia (lack of blood) can manifest in unexpected and serious ways. In this article, we’ll explore anatomy, causes, symptoms, diagnosis, treatments, complications, and practical advice for patients.
Anatomy & Function: Why the Subclavian Artery Matters
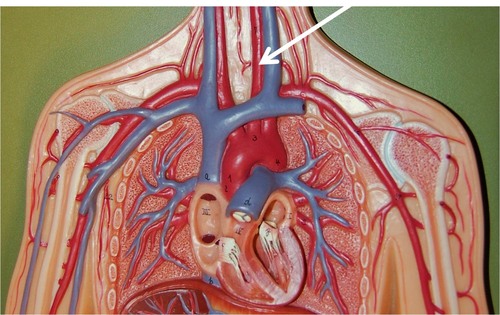
To understand subclavian artery disease, it helps to recall the role of the subclavian vessels:
-
The subclavian arteries (left and right) are major arteries that deliver oxygenated blood from the heart (via the aorta or brachiocephalic trunk) to the upper limbs, portions of the neck, shoulder, and parts of the chest wall.
-
The subclavian arteries also give off branches such as the vertebral artery, which contributes to the blood supply of the brain (particularly the posterior circulation), and other branches to the chest and shoulder girdle.
-
Because of this branching, a blockage in the proximal subclavian artery (i.e., before the vertebral branch) can lead to blood flow being diverted (“stolen”) from the vertebral artery toward the arm, a phenomenon known as subclavian steal syndrome.
In short: the subclavian arteries do more than just serve the arm — they are part of the vascular network that supports both limb function and brain perfusion.
What Is Subclavian Artery Disease?
Subclavian artery disease generally refers to stenosis (narrowing) or occlusion (complete blockage) of the subclavian artery. The most common cause is atherosclerosis (plaque buildup). Other possible causes include:
-
Thrombosis (formation of a clot within the artery)
-
Vasculitis (inflammation of the arterial wall)
-
Fibromuscular dysplasia or nonatherosclerotic vascular disease
-
Radiation-induced arterial injury (in patients who previously had chest radiation)
-
Anatomical compression (e.g. thoracic outlet syndrome) causing external pressure on the vessel
-
Congenital anomalies (less commonly)
Because many cases develop slowly and the body often compensates via collateral circulation (alternate pathways), some patients never develop obvious symptoms.
However, when the narrowing becomes significant or the compensatory mechanisms are insufficient, clinical manifestations can emerge.
Clinical Presentation: Symptoms & Signs
What a patient experiences depends on how severe the blockage is, its location relative to branch points (especially the vertebral artery), and how well collateral circulation can compensate. Some common features include:
Arm / Upper Limb Symptoms (Ischemia)
-
Claudication of the arm: pain, fatigue, cramping or heaviness in the arm or hand during use, especially when lifting the arm or during exertion.
-
Numbness, tingling, paresthesia in the affected arm or hand.
-
Rest pain or discomfort even without exertion, in more severe disease.
-
Coolness or pallor of the hand or fingers, or changes in skin color (e.g. blueness) due to inadequate perfusion.
-
Weakened or diminished pulses in the affected arm. On physical exam, the pulse may be weaker or delayed compared to the opposite side.
-
A significant difference in blood pressure between the two arms (often > 10–20 mm Hg) may be a clue.
Cerebrovascular / Vertebrobasilar Symptoms (Steal Phenomenon)
When the subclavian lesion is proximal to the vertebral artery, blood meant for the brain may be diverted to the arm during exertion — this is subclavian steal syndrome. Symptoms may include:
-
Dizziness, vertigo, or lightheadedness, especially during arm exertion or with head turning
-
Fainting or syncope in extreme cases
-
Blurred vision, visual disturbances
-
Ataxia, imbalance, gait changes or coordination problems
-
In rare settings, symptoms of cerebral ischemia or transient ischemic attacks (TIAs) may arise if the diversion is significant.
Because many patients are asymptomatic or slowly compensated, the syndrome can be underdiagnosed.
Other Manifestations & Red Flags
-
In some patients, embolization (a piece of plaque or clot breaking off) can lead to finger or hand ischemia.
-
Coronary steal syndrome in patients who have had a coronary bypass graft using an internal mammary artery — if the subclavian artery supplying that graft becomes stenosed, blood may be diverted away from the heart.
-
Worsening of symptoms with time, or worsening neurological symptoms, should prompt urgent evaluation.
Diagnostic Evaluation
If a clinician suspects subclavian artery disease, the diagnostic approach typically includes:
Physical Examination & Bedside Clues
-
Measure blood pressure in both arms, compare them (a difference > 10–15 mm Hg is suggestive).
-
Palpate and compare pulses in both arms (radial, brachial).
-
Auscultate for a bruit (a whooshing sound over the subclavian region) that may indicate turbulent flow.
-
Look for signs of poor perfusion: coolness, pallor, delayed capillary refill in the hand/fingers.
-
Check for neurologic signs or symptoms (dizziness, imbalance) that may hint at vertebrobasilar insufficiency.
Noninvasive Imaging & Vascular Studies
-
Doppler ultrasound / duplex scan of the subclavian and vertebral arteries to assess flow velocity, direction, and presence of stenosis.
-
CT angiography (CTA) or MR angiography (MRA) to visualize the arterial anatomy and detect narrowing, occlusions, and collateral pathways.
-
Digital subtraction angiography (DSA) (invasive angiogram) is often considered the gold standard and can also allow endovascular intervention at the same time.
In many settings, noninvasive imaging suffices for planning interventional treatment.
Ancillary Testing & Risk Factor Workup
Because subclavian arterial disease often goes hand in hand with generalized atherosclerosis, the workup should include:
-
Lipid profile, glucose / HbA1c
-
Blood pressure measurement and assessment / control
-
Assessment of smoking status, lifestyle, diet
-
Other vascular imaging (if suspicion of peripheral vascular disease, carotid disease, coronary disease)
This comprehensive evaluation helps guide both acute intervention and long-term secondary prevention.
Treatment Approaches & Strategies
Management of subclavian artery disease depends on symptoms, severity, comorbid conditions, and the feasibility of intervention. Broadly, therapies fall into medical (conservative) and revascularization (endovascular or surgical) categories.
Medical & Conservative Therapy
For patients who are asymptomatic or have mild symptoms, initial management often targets the underlying vascular disease and risk factors:
-
Antiplatelet therapy, such as aspirin (or sometimes clopidogrel), to reduce the risk of clot formation.
-
Statin therapy or other lipid-lowering agents to manage atherosclerotic burden.
-
Control of hypertension, diabetes, and other cardiovascular risk factors (diet, exercise, smoking cessation).
-
Lifestyle modifications: weight control, regular exercise, dietary changes (low in saturated fats), and avoidance of tobacco.
-
Close clinical monitoring: periodic assessment of arm symptoms, blood pressure differences, and surveillance imaging (especially if disease progresses).
However, medical therapy is typically supportive rather than curative. If symptoms worsen or the disease becomes disabling, revascularization is considered.
Endovascular Intervention (Angioplasty & Stenting)
Over the past decades, endovascular therapy has become the first-line interventional approach for many patients with symptomatic subclavian arterial disease. Its advantages include being less invasive, shorter hospital stay, and lower procedural risk compared to open surgery.
Procedure Highlights:
-
A guidewire is navigated across the narrowed segment, then a balloon is inflated (angioplasty) to dilate the vessel.
-
In most cases, a stent is deployed to maintain patency and prevent recoil or restenosis.
-
The technical success rates are high (often in the 90+% range) and complication rates are relatively low.
-
In one study, endovascular procedures succeeded in 96% of cases with a 3-year patency rate of 92%.
-
However, in long or completely occluded lesions, or when the lesion cannot be crossed with a wire, limitations exist, and surgical options may be necessary.
After stent placement, dual antiplatelet therapy (e.g. aspirin + clopidogrel) is often used for 6–12 months, followed by single antiplatelet therapy long term.
Surgical / Open Revascularization
When endovascular intervention is not feasible or fails (due to complex anatomy, heavy calcification, inability to cross occlusions), open surgical procedures are considered. Options include:
-
Carotid–subclavian bypass: using a synthetic graft from the carotid to the subclavian artery.
-
Subclavian artery transposition: reattaching the subclavian artery to the carotid artery.
-
Axillo-axillary bypass: connecting the two axillary arteries (bypassing the subclavian) using graft.
-
Endarterectomy: surgical removal of plaque from the artery (less common in subclavian lesions).
Open surgery usually offers better long-term durability and lower restenosis rates, but with more risk, longer recovery, and higher invasiveness.
Hybrid Approaches & Decision Making
In many advanced vascular centers, a hybrid approach combines the best of endovascular and open techniques. Decisions are based on:
-
Lesion type, length, complexity
-
Patient’s comorbidities and surgical risk
-
Operator and center expertise
-
Urgency and severity of symptoms
When endovascular methods aren’t successful or durable, surgical bypass or transposition is the fallback.
Prognosis, Follow-Up, and Complications
Outcomes & Patency
-
Success rates of angioplasty + stenting are high (90+%) with low complication rates.
-
Long-term patency is good: e.g., 92% at 3 years in one cohort.
-
Surgical bypass/transposition often maintains excellent patency over 5–10 years.
-
Restenosis is a risk in stented segments; reported rates vary (e.g. 6%–21% in some series)
Monitoring & Follow-Up
-
After intervention, regular follow-up is essential. Blood pressure comparisons, duplex scans, and clinical evaluation help detect restenosis early.
-
Suggested follow-up intervals: 3–6 months in the first year, then annually.
-
Loss of pressure or worsening symptoms may be early signs of re-narrowing.
-
Continuation of antiplatelet therapy, lipid control, blood pressure and diabetes management are integral to long-term success.
Potential Complications & Risks
-
Bleeding, hematoma, or vascular injury during intervention
-
Stroke or transient ischemic attack (particularly with proximal arterial interventions)
-
Stent re-occlusion or in-stent restenosis
-
Graft failure or infection (in surgical cases)
-
Nerve injury (e.g. brachial plexus or sympathetic chain) during surgery
Despite these risks, in experienced hands and properly selected patients, outcomes are favorable, and symptom relief is commonly achieved.
Prevention & Risk Reduction
Because subclavian artery disease is often part of broader atherosclerosis, prevention focuses on mitigation of cardiovascular risk. Key steps include:
-
Smoking cessation
-
Healthy diet: low in saturated fats, trans fats, and cholesterol
-
Regular physical activity
-
Control of hypertension, diabetes, and dyslipidemia
-
Statin therapy and antiplatelet therapy as indicated
-
Routine cardiovascular evaluation (especially if other vascular disease is known)
-
Managing body weight, stress, and adopting healthy lifestyle behaviors
Such measures not only reduce risks specific to subclavian disease but also lower the overall burden of cardiovascular events.
When to See a Specialist — Red Flags & Recommendations
You should consider evaluation by a vascular specialist (vascular surgeon, interventional radiologist, or cardiologist) if:
-
You experience unexplained arm pain, fatigue, or weakness, especially with exertion or elevation
-
There is a notable difference in blood pressure between your arms
-
You have dizziness or neurologic symptoms linked to arm use
-
You have known vascular disease elsewhere (e.g., in legs or coronary arteries) and risk factors for atherosclerosis
-
You have had a prior coronary bypass using internal mammary artery and new symptoms suggest possible graft compromise
Early diagnosis allows better planning and less invasive treatment, reducing the risk of complications.
Illustrative Patient Scenario
Case Example:
Mrs. Z, a 62-year-old woman with hypertension and hyperlipidemia, began noticing fatigue, tingling, and mild cramping in her left arm when she reached overhead or lifted objects. She also experienced occasional lightheadedness when exercising her left arm. On examination, her left arm blood pressure was 20 mm Hg lower than her right, and a bruit was heard over the left supraclavicular area.
A duplex ultrasound showed increased velocity and signs of stenosis in the left proximal subclavian artery; an MRA confirmed a ~70% narrowing just proximal to the vertebral artery takeoff. Given her symptoms (upper limb claudication plus vertebrobasilar symptoms), she was referred for intervention. An angioplasty with stenting was performed, restoring antegrade flow. Her arm symptoms resolved, and her dizziness improved. She was placed on dual antiplatelet therapy for 6 months, and followed with duplex scans over the next years.
This case exemplifies how timely recognition and management can restore function and prevent further ischemic damage.
Key Takeaways & Closing Thoughts
-
Subclavian artery disease is a condition in which narrowing or blockage impairs blood flow to the arm and potentially “steals” flow from the vertebral artery.
-
Many cases remain asymptomatic due to collateral circulation, but when symptoms arise (arm claudication, neurological signs), they can be significant.
-
Diagnosis hinges on both simple clinical clues (blood pressure difference, pulse exam) and imaging studies (duplex, CTA/MRA, angiography).
-
Endovascular therapy (angioplasty + stenting) is the preferred first-line treatment for most symptomatic patients, offering high success rates and low complication risk.
-
Surgical revascularization (bypass, transposition) remains important when endovascular options fail or are not feasible.
-
Because subclavian artery disease usually coexists with systemic vascular disease, managing underlying risk factors is essential.
-
Long-term follow-up, surveillance, and adherence to medical therapy are crucial to lasting success.
At Big Apple Medical Care, we take vascular health seriously. If you or someone you know has unexplained arm symptoms, dizziness, or suspicious blood pressure differences, don’t delay evaluation. Early diagnosis and intervention can prevent further complications, restore limb function, and preserve neurological health. Reach out to our vascular team to schedule a consultation or further diagnostic evaluation.