At Big Apple Medical Care, our mission is to deliver authoritative, up-to-date medical insight that empowers patients and their families. In this article, we explore how advances in diagnosis, surgical technique, chemotherapy, radiation, surveillance, and personalized therapies have transformed testicular cancer from a once-deadly disease into one of the most curable cancers in men today.
Introduction: The Transformation of Testicular Cancer Treatment
Decades ago, a diagnosis of metastatic testicular cancer often meant a grim prognosis. In the early 1970s, survival rates for patients with metastatic disease hovered around 5 %.
Today, thanks to breakthroughs in medical science, five-year survival rates for testicular cancer across all stages exceed 95 %.
This dramatic improvement is not the result of a single innovation, but rather the cumulative impact of many advances: earlier detection, refined surgery, more effective and less toxic chemotherapy, tailored radiation strategies, improved supportive care, and use of surveillance protocols to avoid overtreatment. In many ways, testicular cancer has become a model for successful cancer therapy.
In this article, we examine how each of these modern strategies plays a role in maximizing cure rates, minimizing side effects, and optimizing patient quality of life.
Epidemiology, Risk Factors, and Early Detection
Epidemiology and Risk
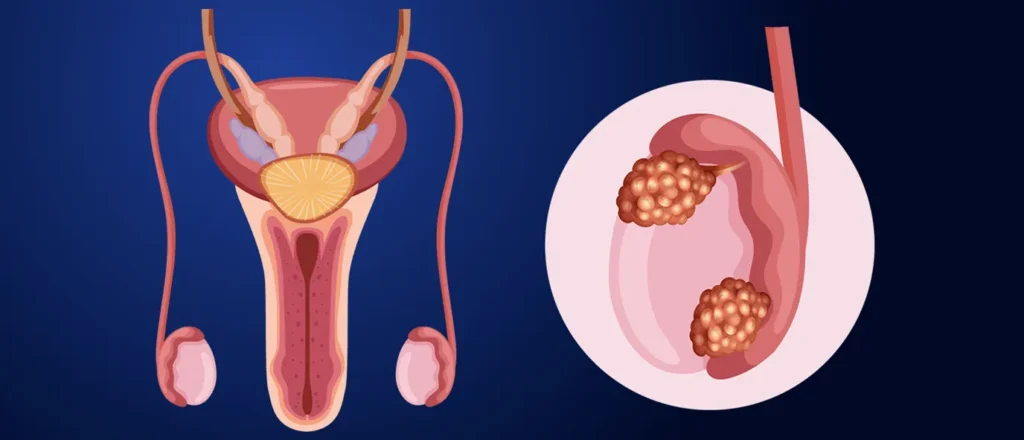
Testicular cancer is relatively uncommon, constituting about 1 % of male cancers, but it is the most common cancer in men aged 15 to 45.
Risk factors include:
-
Cryptorchidism (undescended testicle)
-
Personal or family history of testicular cancer
-
Testicular atrophy or prior testicular injury
-
Certain genetic predispositions
Because the disease typically affects younger men with otherwise long life expectancy, effective, low-toxicity therapies and fertility preservation are especially important.
Early Detection and Self-Examination
One of the most powerful contributors to high cure rates is early detection. Many testicular cancers present as a painless lump or swelling in the testicle. Monthly testicular self-examination (TSE) can help detect changes earlier. While there is no universal consensus on TSE, in high-risk individuals or those with suspicious findings, early evaluation is key.
When diagnosis occurs while disease is still localized, cure rates approach 99 %.
Modern Diagnostic and Staging Approaches
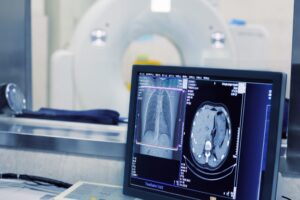
Accurate diagnosis and staging are foundational to selecting the optimal therapy and avoiding unnecessary treatment:
-
Physical examination and testicular ultrasound to confirm intratesticular masses.
-
Serum tumor markers: AFP (alpha-fetoprotein), β-hCG (beta-human chorionic gonadotropin), and LDH (lactate dehydrogenase). These help classify tumor type (seminoma vs nonseminoma), guide staging, monitor response, and detect recurrence.
-
Imaging (CT scans of abdomen, pelvis, chest) to assess lymph node involvement and distant metastases.
-
Pathology evaluation after surgical removal, to classify tumor histology, assess risk factors, and inform further therapy.
The tumor classification into seminoma and nonseminoma is crucial, since each behaves differently and responds to therapy differently.
With modern staging and risk stratification, clinicians can tailor therapy—escalating treatment only when needed, and de-escalating when risks are low.
Surgical Advances: Precision, Safety, and Organ Preservation
Radical Inguinal Orchiectomy
The gold-standard first step in nearly all testicular cancer cases is radical inguinal orchiectomy — removal of the affected testicle via an incision in the groin, without violating the scrotum to minimize tumor seeding. This is a relatively safe outpatient procedure in many centers.
Beyond removal, this procedure provides tissue for definitive diagnosis and staging.
Testis-Sparing Surgery (Partial Orchiectomy)
In selected patients with small masses (often < 20 mm), partial orchiectomy (testis-sparing surgery) may be considered, especially when tumor markers are negative and imaging suggests low malignancy risk. This approach can help preserve hormonal function and fertility, but is used only in carefully selected cases.
Retroperitoneal Lymph Node Dissection (RPLND)
For nonseminoma cases or in settings of residual nodal disease, modern RPLND techniques have been refined to reduce complications while achieving excellent control.
Minimally invasive and nerve-sparing RPLND variants help preserve ejaculatory function and reduce morbidity.
Over time, surgical techniques have improved with better imaging guidance, intraoperative mapping, and less invasive dissection protocols, thereby reducing complication rates while preserving oncologic safety.
Chemotherapy Revolution: Cisplatin and Beyond
The single greatest leap in testicular cancer curability came with the development of cisplatin-based chemotherapy regimens, particularly the BEP regimen (Bleomycin, Etoposide, and cisPlatin). This innovation transformed survival even in metastatic disease.
Effective Combination Regimens
Modern protocols tailor the number of cycles and drug doses based on risk stratification (good, intermediate, poor prognosis). In favorable-risk disease, two to three cycles may suffice; in more advanced disease, more intensive regimens are used.
-
Dose optimization to maximize tumor kill and minimize toxicity
-
Use of growth factor support and supportive care to allow safe dosing
-
Better hydration and protective protocols to mitigate kidney and hearing damage
-
Salvage and high-dose chemotherapy with stem-cell rescue in refractory or relapsed disease
Through these refinements, even relapsed patients often achieve remission.
Radiation Therapy: Precision and Selectivity
Radiation therapy plays a more limited but still valuable role, especially in seminoma:
-
In stage I seminoma, adjuvant carboplatin has largely supplanted radiation in many protocols, reducing long-term radiation-associated risks.
-
In nodal seminoma (stage II), targeted radiotherapy to retroperitoneal lymph nodes continues to be a standard option.
-
Advanced image-guided radiation techniques help minimize dose to nearby organs, thereby reducing toxicity.
Because radiation carries late risks (secondary malignancies, cardiovascular effects), modern strategies reserve it for circumstances where benefits outweigh long-term risks.
Surveillance and Risk-Adapted Strategies
One of the most significant innovations in modern testicular cancer care is active surveillance — monitoring patients closely rather than applying adjuvant therapy to all.
For low-risk stage I seminoma or nonseminoma, surveillance is now often the preferred initial approach.
Surveillance protocols typically include regular imaging and tumor marker checks every few months, with the option to intervene if recurrence occurs.
This strategy spares many men from unnecessary chemotherapy or radiation and reduces treatment-related toxicity and long-term side effects.
When risk factors (e.g. lymphovascular invasion, high markers) are present, adjuvant therapy is considered, balancing risk of relapse and overtreatment.
Fertility Preservation, Survivorship, and Quality of Life
Because testicular cancer affects younger men, preserving fertility, hormonal function, and long-term health is paramount.
Sperm Banking
Before initiating treatments (especially chemotherapy or radiation), patients are routinely counseled about sperm cryopreservation. This gives men the option of future conception. Although many men recover spermatogenesis, treatment effects on fertility can persist.
Minimizing Toxicity
Modern regimens, dose reductions, and supportive care (e.g., hydration, protective agents) help reduce risks of nephrotoxicity, ototoxicity, neuropathy, and pulmonary effects.
Long-Term Monitoring
Survivorship includes surveillance for late effects — such as second cancers, cardiovascular disease, metabolic changes, and endocrine dysfunction — and psychosocial support.
Quality of Life and Psychosocial Support
Many survivors lead robust, full lives. Yet emotional support, fertility counseling, sexual health, and monitoring for anxiety or depression are key elements of holistic care.
Outcomes and Prognosis: Numbers That Inspire
Thanks to modern treatments, testicular cancer has one of the most remarkable success stories in oncology.
-
Localized disease: 5-year survival ~ 99 %
-
Regional spread: ~ 96 % 5-year survival
-
Distant metastases: Even in metastasis, survival rates may be ~ 72 % or higher depending on risk and treatment response.
-
Overall, close to 95 % or more of men with testicular cancer survive long-term.
These statistics do not capture individual variation. Factors that influence outcome include:
-
Stage at diagnosis
-
Tumor type (seminoma vs nonseminoma)
-
Tumor marker levels
-
Response to therapy
-
Patient comorbidities and treatment tolerance
Nevertheless, the bottom line is clear: testicular cancer is among the most curable solid malignancies in modern medicine.
Future Directions & Innovations
While current approaches are highly effective, research continues to refine and improve:
-
Targeted therapies and molecular profiling to tailor treatments more precisely
-
Immunotherapy exploration (though currently limited in testicular cancer)
-
Reduced-toxicity regimens to further protect fertility and reduce late effects
-
Circulating tumor DNA / liquid biopsies for earlier detection of relapse
-
Long-term survivorship programs that integrate cardiovascular care, lifestyle interventions, and psychological support
Clinical trials remain critical, and many leading institutions now offer novel therapeutic options embedded in research protocols.
Conclusion: A Legacy of Hope and Excellence
At Big Apple Medical Care, we believe the story of testicular cancer treatment is a beacon of what oncology can achieve when scientific rigor, innovation, and patient-centered care converge.
The journey from near-hopelessness to 95 %+ cure rates illustrates not just technical success, but the potential for medicine to restore life, hope, and futures. Every man diagnosed with testicular cancer today has access to treatments that not only aim for survival, but also prioritize fertility, function, and long-term well-being.
If you or a loved one is facing a testicular cancer diagnosis, know that you are part of a medical narrative marked by progress, precision, and promise. With early detection, expert multidisciplinary care, and ongoing advances, many men go on to full, vibrant lives.