Vein issues are a common concern during pregnancy. Many expectant mothers experience varicose veins, spider veins, vulvar varicosities, or hemorrhoids. While these problems are often benign and sometimes temporary, they can cause discomfort, and in certain situations, require medical attention. At Big Apple Medical Care, we believe in empowering our patients with knowledge: what causes these vein issues, how they’re managed during pregnancy, and what removal or treatment options are available once it’s safe.
Why Are Vein Issues So Common During Pregnancy?
Pregnancy induces a host of hormonal, mechanical, and circulatory changes that make vein problems more likely. Key causes include:
-
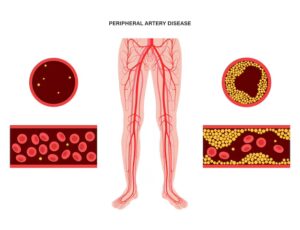
Increased Blood Volume & Circulatory Load
To support the placenta and growing fetus, an expecting mother’s blood volume increases by up to 50%.This expansion increases pressure on veins, particularly in the legs and pelvis. -
Hormonal Changes
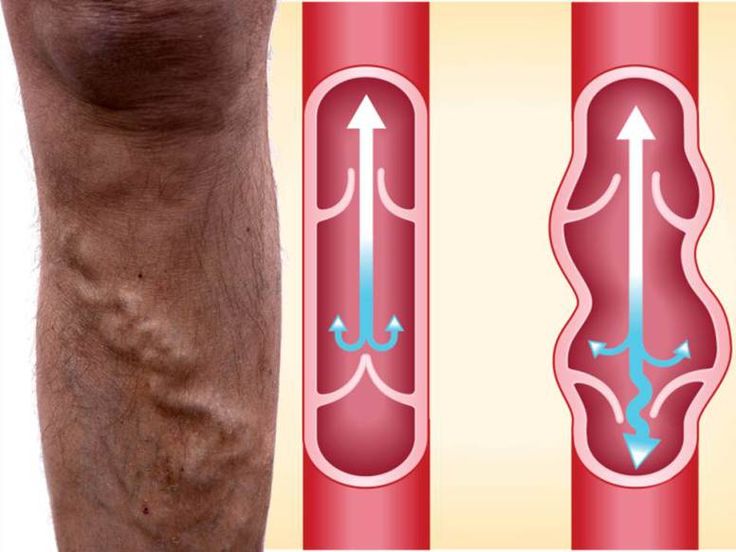
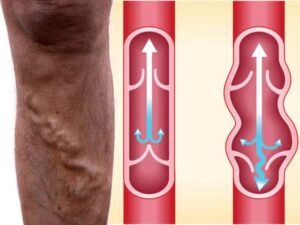
Elevated levels of hormones such as progesterone cause the vein walls to relax, reducing tone and allowing veins to widen. At the same time, vein valves may become less efficient, permitting blood to pool rather than flow smoothly back toward the heart. -
Mechanical Pressure from the Uterus
As the uterus expands, it presses on the pelvic veins and the large central vein (inferior vena cava). This pressure impedes blood return from the legs, contributing to venous stasis (slowing of blood flow) and increased risk of bulging veins or swelling. -
Genetic Predisposition and Other Risk Factors
• Family history of varicose veins increases your risk.
• Multiple pregnancies tend to exacerbate the issue; each pregnancy can further stretch veins and reduce valve efficacy.
• Excess weight gain increases pressure on leg veins.
• Prolonged standing or sitting also plays a role in worsening symptoms. -
Hormonal Influence on Vein Tone & Fluid Retention
Pregnancy hormones promote fluid retention, which can increase swelling (edema) in the legs and accentuate visible vein issues. The relaxing of vessel walls due to hormonal influence also makes veins more likely to dilate under increased pressure.
Common Types of Vein Problems During Pregnancy
These are the most frequent vein-related conditions that pregnant women may notice:
| Condition | Description | Typical Locations & Symptoms |
|---|---|---|
| Varicose Veins | Swollen, twisted veins that bulge under the skin; often blue or dark purple in appearance. | Legs (calves, thighs), ankles; sometimes vulva (vulvar varicosities). Symptoms: heaviness, aching, visible bulging, cramps, itchy or burning sensation. |
| Spider Veins | Smaller, thin lines, red or blue, that appear close to skin’s surface. | Legs commonly, sometimes thighs. Usually cosmetic, but may accompany discomfort or swelling. |
| Vulvar Varicosities | Enlarged veins in the vulva or genital area. | Vulva; symptoms include discomfort, swelling, heaviness, sometimes visible bulging. |
| Hemorrhoids | Varicose veins in the rectal or anal area. | Anal canal/rectum; symptoms include itching, pain, possibly bleeding. Associated with constipation, straining. |
Symptoms and When Vein Changes Need Attention
While many vein issues in pregnancy are mild and self-limiting, it’s important to know what symptoms may need medical evaluation. Common symptoms include:
-
Aching, heaviness, or pain in the legs, especially after standing or sitting for long durations.
-
Swelling (edema) of legs, ankles, especially toward the end of the day.
-
Leg cramps, especially at night.
-
Itching, burning, or irritation over bulging veins.
-
Bleeding or ulceration near varicose veins (rare but concerning).
-
Redness, warmth, or swelling, especially in one leg — these could indicate a clot (superficial thrombophlebitis or deeper clot). Seek medical help immediately.
Symptoms that resolve after childbirth are common. However, if vein issues persist beyond ~6–12 months postpartum, or are severe during pregnancy, more proactive treatment may be needed.
Safe Management During Pregnancy
Because many vein problems will improve after delivery, the approach during pregnancy is often conservative and focused on symptom relief. Interventional or removal procedures are usually postponed until after delivery. Here are safe management strategies:
-
Compression Therapy
Wearing properly fitted compression stockings or support hose helps by gently pressing on veins, reducing pooling of blood, lowering swelling, and easing symptoms. A standard recommendation in guidelines. -
Leg Elevation & Mobility
Elevate legs above heart level whenever possible to reduce venous pressure. Avoid standing or sitting for long periods without moving. When you sit, avoid crossing legs. Walking or gentle prenatal exercise helps circulation. -
Sleep Positioning
Lie on the left side to reduce pressure from the uterus on the inferior vena cava, facilitating more efficient blood return from your legs. -
Dietary Measures & Lifestyle
-
Reduce sodium to limit fluid retention and swelling.
-
Eat plenty of fiber to prevent constipation, which worsens hemorrhoids and varicose veins.
-
Maintain healthy weight gain within recommended guidelines.
-
Stay hydrated.
-
Wear loose clothing (avoid tight waistbands or clothes constricting groin/legs).
-
-
Comfort Measures
-
Use cold compresses for discomfort.
-
Sitz baths for hemorrhoids.
-
Leg massage or gentle stretching.
-
-
Monitoring & Safety
If you notice signs of deep vein thrombosis (severe swelling, pain, warmth, redness), bleeding, or ulcers, contact your healthcare provider immediately. Doppler ultrasound may be used in certain cases to assess blood flow.
Removal and Surgical Options
Most removal or interventional treatments are deferred until after pregnancy and breastfeeding, unless symptoms are severe or complications arise. Once safe, several options exist. Here are some of the removal or treatment methods, their suitability, risks, and what to consider.
| Treatment Option | What It Involves | When It’s Suitable | Risks / Considerations |
|---|---|---|---|
| Sclerotherapy | A chemical (liquid or foam) is injected into small-to-medium sized varicose or spider veins; causes vein wall scarring and closure, after which vein gradually fades. | Post-partum / when you are not pregnant or nursing; smaller varicose veins or spider veins. Good for cosmetic and symptom relief. | Possible bruising, mild pain, risk of allergic reaction; requires compression afterward. Not usually done during pregnancy. |
| Endovenous Thermal Ablation (EVLA / Radiofrequency Ablation) | A catheter delivers heat (laser or radiofrequency) to the inside of the diseased vein, causing closure. | For larger varicose veins (like saphenous vein reflux), post-pregnancy; when symptoms persistent or quality of life affected. | Requires anesthesia/local numbing; risk of skin burns, nerve damage, or pigment changes. Recovery includes wearing compression. |
| Ambulatory Phlebectomy | Micro-incisions are made to remove bulging veins on the skin surface. | Smaller, surface varicose veins not suitable for ablation; post-delivery. | Minor scarring, wound care; possible residual discomfort. |
| Vein Adhesive (e.g., VenaSeal) | Medical adhesive used to seal off problematic veins through a catheter; no heat required. | In situations where patient prefers non-thermal methods and for suitable vein types. Post-pregnancy. | |
| Foam Varithena® Treatment | A foam sclerosant is injected into larger varicose veins to cause closure. | Selected larger vein segments; again, after pregnancy. | |
| Ligation and Stripping Surgery | Traditional surgical removal of a vein segment; involves tying off (ligation) and pulling out (stripping). | Severe varicose disease when less invasive techniques are inadequate; after pregnancy and when patient is fully healed postpartum. | Greater recovery time; higher risk of complications; scarring potential; more downtime. |
Timing: When to Do Removal vs When to Wait
-
During pregnancy: In almost all cases, interventional or removal treatments are postponed until after childbirth. The reason: risk to fetus, risk of infection, anesthesia concerns, changes in venous pressure that may reverse some changes naturally after delivery.
-
Postpartum / Breastfeeding period: Many veins improve significantly within 6-12 weeks after delivery. For persistent symptoms, you may evaluate treatment options. The optimal timing is generally several months after childbirth, when body’s hormonal, fluid, circulatory systems are returning to pre-pregnancy state.
Prevention and Long-Term Vein Health
Even though some risk factors are unavoidable during pregnancy, you can take steps to minimize severity, prevent worsening, and preserve long-term vein health.
-
Move frequently: Walk, stretch, change positions — avoid long periods of standing or sitting.
-
Exercise regularly: Prenatal exercise, yoga, swimming facilitate blood flow.
-
Use compression stockings early: If you notice swelling or vein changes, begin using compression garments to prevent progression.
-
Maintain ideal weight gain: Follow obstetrician’s guidelines; excess gain increases pressure on veins.
-
Nutrition: High fiber to avoid constipation, low salt to reduce fluid retention, adequate hydration.
-
Proper posture: Avoid crossing legs; elevate legs when resting; avoid constrictive clothing.
-
Skin care: Moisturize skin over varicosities to reduce itching; avoid injury to bulging veins.
Risks If Vein Issues Are Left Unmanaged
While many pregnancy-related vein issues are benign, severe or unmanaged cases may lead to:
-
Persistent pain and discomfort, limiting mobility and quality of life.
-
Skin changes: swelling, skin discoloration, ulceration near affected veins.
-
Bleeding, especially in vulvar or hemorrhoid varicosities.
-
Superficial or deep vein thrombosis (DVT): particularly in cases with swelling, redness, warmth, or pain. Untreated DVT can lead to serious complications.
Consultation & Diagnostic Approaches
If you are pregnant and have vein issues, or postpartum and symptoms persist, clinical evaluation may include:
-
Physical exam of legs, vulva, rectal area if hemorrhoids.
-
Evaluation of symptoms: severity, duration, whether symptoms worsen with standing, night, etc.
-
Doppler ultrasound of leg, pelvis, or vulvar veins to assess blood flow, valve competency, extent of reflux.
-
Measurement of residual urine in bladder in hemorrhoid / vulvar swelling cases (for symptom correlation).
-
Assessment of patient’s medical history, family history, co-morbidities (e.g., clotting disorders).
How Big Apple Medical Care Helps
At Big Apple Medical Care, our approach to managing vein issues in pregnancy and thereafter is grounded in safety, symptom relief, and individualized care.
-
Comprehensive Evaluation
We assess your symptoms, medical history, risk factors, and inspect veins both under pressure (standing) and at rest. If needed, we arrange Doppler ultrasound imaging. -
Conservative Management First
Our initial strategy during pregnancy includes compression therapy, posture and dietary modifications, supportive garments, and lifestyle guidance to reduce venous pressure and symptoms. -
Close Monitoring
We keep track of how symptoms evolve, ensure no warning signs of thrombosis, bleeding, or severe swelling. -
Post-Delivery Treatment Planning
Once you have delivered and it is safe, we discuss removal or interventional options suitable for your condition, vein type, severity, and cosmetic concerns. We help you weigh benefits and risks of surgical vs minimally invasive methods. -
Patient Education & Support
Understanding what is normal, what to watch out for, and when to seek help is central. We also provide support for managing discomfort, improving mobility, and preventing progression in future pregnancies.
Key Takeaways
-
Vein issues—varicose veins, spider veins, vulvar varicosities, hemorrhoids—are common during pregnancy due to hormonal changes, increased blood volume, pressure from the growing uterus, and genetic predisposition.
-
Most vein problems improve on their own after childbirth, often within 6-12 weeks. During pregnancy, treatment focuses on symptom relief and preventing complications.
-
Removal or interventional treatment options (sclerotherapy, ablation, phlebectomy, vein adhesive, etc.) are typically deferred until after pregnancy and breastfeeding.
-
Preventive steps and conservative measures can reduce discomfort and the severity of vein issues.
-
Persistent or severe cases, symptoms suggesting clot, bleeding, or ulceration warrant evaluation by a vascular or vein specialist.
At Big Apple Medical Care, we are committed to supporting you through every stage—pregnancy, postpartum, and beyond—to ensure your vein health is managed with care, safety, and respect for your body’s natural healing. If you’re experiencing discomfort, visible varicose veins, or lingering symptoms after pregnancy, we’re here to help you explore safe, effective options that fit your needs and priorities.