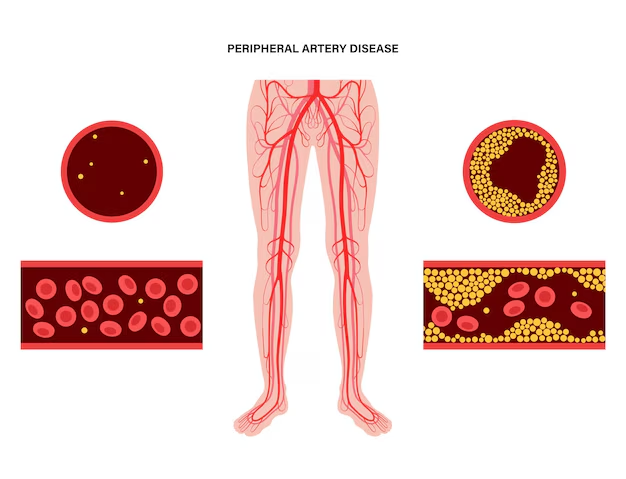
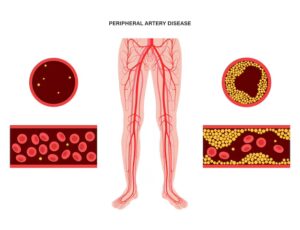
Peripheral artery disease (PAD) is a common and serious vascular condition characterized by narrowing or blockage of arteries outside of the heart, especially in the legs. It reduces blood flow, causes symptoms like leg pain (claudication), slows walking, wounds heal poorly, and increases risks of cardiovascular events. Many patients wonder: can Peripheral artery disease be reversed naturally, without surgery or invasive procedures?
While full “reversal” (i.e., removing all atherosclerotic plaques) is rarely realistic in advanced disease, research increasingly shows that natural measures — lifestyle, diet, exercise, quitting tobacco — can slow progression, reduce symptoms, improve walking ability, and in some early cases, partially reverse vascular damage or restore function. Here we explore what the science says, what is possible, what limitations exist, and how Big Apple Medical Care can guide patients toward the best natural strategies.
Understanding PAD: What “Reversal” Means
Before exploring whether PAD is reversible, it helps to clarify what “reversal” means in this context:
-
Symptom improvement / remission: Reduced leg pain, longer walking distance, fewer ulcers, better quality of life.
-
Stabilization: Halting or slowing further progression of arterial narrowing or blockages.
-
Partial physiological improvement: Improved endothelial function, reduced inflammation, better circulation, improved collateral blood flow.
-
Structural change: This is harder—reducing the plaque size is difficult once advanced, but early disease may allow some regression of fatty streaks or soft plaque.
Full cure of PAD (i.e., restoring arteries to entirely normal anatomy) is seldom possible, especially in moderate or severe disease. However, substantial benefit from non-surgical, “natural” interventions is well supported — especially when started early.
Key Natural Measures That Experts Agree Can Help
Researchers and guideline bodies emphasize several non-invasive measures as first-line interventions for PAD. These are backed by studies showing measurable improvements in symptoms, vascular health, and risk profiles. The main pillars are:
-
Smoking Cessation
-
Smoking is one of the strongest modifiable risk factors for PAD. It contributes to plaque formation, endothelial dysfunction, vasoconstriction, oxidative stress.
-
Quitting smoking reduces progression, improves walking distance, lowers risk of cardiovascular events. Some studies show that former smokers fare much better than current smokers in terms of symptom severity and mortality.
-
-
Regular Exercise, Especially Supervised Walking Programs
-
Walking is considered a cornerstone of PAD management. The “stop-and-start” or interval walking strategy (walk until pain or discomfort, rest, then repeat) improves leg muscle metabolism, stimulates collateral vessel growth, improves exercise tolerance.
-
Supervised exercise therapy (SET) is shown to outperform self-guided walking in many trials. It improves walking distance, quality of life, and functional capacity.
-
-
Dietary Changes
-
Diets rich in anti-inflammatory foods, fiber, lean proteins, whole grains, nuts, seeds, vegetables, fruits are beneficial. Such diets help lower cholesterol, improve endothelial health, reduce oxidative stress.
-
Specific patterns such as the Mediterranean diet and DASH diet (Dietary Approaches to Stop Hypertension) are strongly recommended to manage risk factors (blood pressure, cholesterol) which are major drivers of PAD.
-
-
Weight Management and Control of Risk Factors
-
Maintaining healthy body weight helps reduce inflammatory burden, lowers mechanical stress, improves metabolic health (blood sugar, lipid profile). Obesity exacerbates PAD symptoms and progression.
-
Control of co-morbid conditions: hypertension, hyperlipidemia, diabetes. Proper management via diet, medication when needed, monitoring. These are essential for slowing disease.
-
-
Other Lifestyle Measures
-
Avoidance of sedentary behaviour; increasing daily physical activity beyond walking (e.g. cycling, swimming).
-
Foot care, especially in patients with diabetes or reduced blood flow, to avoid ulcers or infections.
-
Possibly supplementation with nutrients / antioxidants in certain contexts (under medical supervision). Some studies look at vitamin C, E, possibly others — though evidence is less uniform.
-
What the Research Shows: Can Natural Measures Reverse PAD or Improve Outcomes?
Let’s look at what clinical trials and systematic reviews have found regarding “reversal” or improvement.
-
A systematic review titled “Management of Peripheral Arterial Disease: Lifestyle …” (2022) found that lifestyle alterations such as smoking cessation, dietary modifications, and exercise training are essential components. These interventions can lead to improved walking performance, reduced symptoms, and better vascular biomarkers.
-
Exercise Rehabilitation experiments (e.g., Hamburg et al.) show that exercise training improves muscle metabolism, increases walking distance, and can restore certain metabolic parameters in leg muscles affected by PAD.
-
Trials combining dietary interventions (such as modified DASH) with exercise (walking programs) show better improvements than exercise alone in vascular inflammation, walking ability, quality of life. For example, the modDASH+Ex project showed promise in improving outcomes compared to standard exercise alone.
-
While many studies document slowing of progression and symptom relief, few prove full anatomical regression (i.e. reduction of pre-existing arterial plaque) in moderate to severe disease. Early PAD (mild to moderate) responds best. Late stages, especially when there is critical limb ischemia or large occlusions, often require interventional therapy. Several sources note that reversal of PAD is not reliably possible once advanced, but “improvement” and remission of symptoms is realistic with sustained effort.
What Experts Say: Guidelines & Official Recommendations
Authoritative bodies (e.g. NHS, American Heart Association) do not claim that PAD can always be completely reversed naturally, but uniformly recommend non-invasive measures as first-line care:
-
The NHS guidelines state: while there is no cure for PAD, lifestyle changes and medication can help reduce symptoms and prevent disease progression. Key lifestyle changes: regular exercise, stopping smoking.
-
Clinical practice recommendations emphasize supervised exercise therapy (walking), control of blood pressure, cholesterol, diabetes, diet modifications.
-
Some vascular centers note that early diagnosis is vital; the earlier these natural measures are applied, the more likely a patient is to see meaningful improvements.
Limitations: When Natural Measures May Not Fully Reverse PAD
To maintain realistic expectations, it is vital to understand the limitations of natural strategies.
-
Stage of disease matters: In mild to moderate PAD, natural measures can yield substantial improvements. In advanced disease (critical limb ischemia, large occlusion, tissue loss), the arterial damage may be too advanced for reversal without surgical/endovascular intervention.
-
Plaque composition: Calcified plaque is more rigid and less likely to regress. Soft, fatty plaques may respond more to diet and lipid-lowering, but complete removal is rare naturally.
-
Extent of arterial narrowing and collateral capacity: Some people possess better collateral circulation than others, allowing compensation. Natural measures improve collateral growth, but cannot always substitute for major mechanical blockages.
-
Adherence is critical: Benefits require long-term, consistent implementation (years). Short-term changes yield limited gains; disease often resumes if risk factors are not controlled.
-
Genetics, age, co-morbidities: Diabetes, renal disease, advanced age, chronic inflammation, genetic predisposition limit potential for “natural reversal.”
A Practical Roadmap: Natural Strategies to Maximize Improvement
At Big Apple Medical Care, we believe in empowering our patients with a structured and evidence-based plan to maximize natural improvements in PAD. Here’s a roadmap that reflects best practices extracted from research and expert guidelines.
| Strategy | What to Do | Expected Benefits |
|---|---|---|
| Quit Smoking Completely | Use behavioural support, nicotine replacement if needed; aim for total cessation. | Slows progression, improves symptoms, lowers cardiovascular risk. |
| Initiate Supervised Exercise Regimen | Start with interval walking (walk until mild pain/discomfort, rest, repeat), 30-60 minutes per session, at least 3-5 times weekly; ideally professionally supervised for first ~3 months. | Increases walking distance, improves leg muscle metabolism, stimulates collateral blood flow. |
| Adopt Heart-Healthy Diet | Focus on Mediterranean / DASH-style diet: high fiber, fruits/vegetables, lean protein, whole grains; limit saturated/trans fats, cholesterol, refined sugars, excess salt. Include omega-3 rich foods. | Improves lipid profile, reduces inflammation, helps with weight control, better vascular health. |
| Manage Blood Pressure, Cholesterol, Diabetes | Regular monitoring; medications as needed; diet and lifestyle interventions; follow up. | Reduced risk of further arterial damage, lowers risk of cardiovascular events. |
| Maintain Healthy Weight and Body Composition | Aim for gradual weight loss if overweight; reduce visceral fat; preserve muscle mass. | Lowers metabolic burden; improves exercise tolerance. |
| Daily Physical Activity Beyond Formal Exercise | Incorporate walking, using stairs, avoid long periods sitting; leg elevation, foot care. | Enhances circulation, prevents complications. |
| Optimize Nutrition and Possibly Supplementation | Vitamins, antioxidants (if deficient), ensure adequate intake of micronutrients; under clinician guidance. Possibly L-arginine or nitrate sources to support endothelial function. | May improve endothelial health, nitric oxide availability, reduce oxidative stress. |
| Stress Management and Sleep | Adequate sleep, controlling stress (meditation, counselling). | Chronic stress and poor sleep increase inflammation, worsen vascular health. |
Case Examples and Realistic Outcomes
Here are some illustrative scenarios showing how natural measures can lead to meaningful changes in PAD:
-
Early-Stage PAD: A patient with mild claudication, no rest pain, minimal occlusion. Implements smoking cessation, starts supervised walking program, adopts Mediterranean diet. After 6 to 12 months: marked improvement in walking distance, less leg discomfort, improved ABI (ankle-brachial index) in some cases, better lab markers (cholesterol, inflammation).
-
Moderate PAD with Co-morbidities: Patient with diabetes, hypertension, PAD with intermittent claudication. Control of blood sugar, aggressive lipid lowering, weight loss, exercise. After 1-2 years: reduced frequency of symptoms, fewer ulcers, more daily activity, better quality of life. Possibly some plaque stabilization; however, anatomical regression likely partial.
-
Advanced PAD / Critical Ischemia: In cases with tissue loss or severe blockage, natural measures help with symptoms, collateral development, prevent progression, improve healing post-intervention, but often require endovascular or surgical intervention for rescue.
What Experts Caution About: Not a Substitute, But a Foundation
While natural strategies are powerful, experts caution that:
-
They are not replacements for medical therapy or interventional treatments when indicated. If symptoms are severe, if there is risk of limb ischemia, infection, or non-healing ulcers, surgical/endovascular options are required.
-
Screening and monitoring matter. Regular follow-ups (ABI tests, imaging if needed) to assess progression.
-
Medication might still be needed — statins, antiplatelet agents, blood pressure medications — even with excellent lifestyle habits. Guidelines support combined approach.
-
Consistency over years is essential; natural improvements may fade if habits lapse.
How Big Apple Medical Care Can Help You
Here’s how we approach PAD management with a natural-centered plan, integrated with medical oversight:
-
Early Detection and Risk Assessment
We screen patients with risk factors (smoking, diabetes, hypertension, family history) for PAD using non-invasive tests (ABI, doppler, symptom questionnaires). -
Customized Exercise Programs
We offer or refer to supervised walking therapy, physical therapy with PAD expertise, to safely build endurance and walking tolerance. -
Nutrition Counseling
Dietitians work with you to build heart-healthy eating patterns, adjust caloric load, reduce harmful fats, emphasize anti-inflammatory foods. -
Support for Smoking Cessation & Lifestyle Change
Coaching, counseling, sometimes pharmacologic support to quit smoking; tools to increase daily activity; stress management. -
Medical Management When Necessary
While emphasizing natural strategies, we also manage hypertension, cholesterol, diabetes, and use medications when evidence supports better outcomes. We monitor labs, imaging, and symptoms. -
Regular Monitoring & Adjustments
Keeping track of walking distance, symptom diary, ABI or imaging when needed. Adjusting plan as patient improves or encounters changes.
Conclusion: What is Possible, What to Expect
-
Yes, many components of PAD are modifiable, and with sustained natural measures, substantial improvement in symptoms, quality of life, walking ability, and risk of cardiovascular events is often achievable.
-
Full anatomical reversal of moderate to severe artery blockages is rare without medical or surgical intervention. But early disease (soft plaques, early narrowing) may exhibit partial regression with lipid lowering, diet, exercise.
-
Lifestyle interventions are not optional; research and guidelines place them as foundational. Without them, medical or surgical treatments are often less effective or sustainable.
-
Expect progress gradually: improvements in symptoms and function begin weeks to months after beginning major changes; measurable vascular improvements might take months to years.
-
You are in control of many modifiable factors: quitting smoking, moving regularly, eating healthfully, managing weight and comorbidities.
At Big Apple Medical Care, we believe in combining evidence-based natural strategies with medical oversight to help you gain maximal benefit. While we may not always promise complete reversal, we can promise meaningful improvement — reduced pain, more mobility, better leg health, fewer complications, improved overall cardiovascular health.