At Big Apple Medical Care, we believe in making diagnoses precise and patient-centered. Uterine fibroids (leiomyomas) are among the most common benign tumors affecting women of reproductive age. While many fibroids cause no symptoms, others lead to heavy periods, pain, fertility problems, or pressure symptoms on bladder and bowel. Correct diagnosis of fibroids—including location, size, number, and relationship to the uterine cavity—is essential to plan treatment that is effective and tailored to each patient.
In this article, we will explain:
-
What fibroids are and why diagnosis matters
-
Clinical evaluation: history + physical exam
-
Laboratory tests
-
Imaging & diagnostic procedures — ultrasound, MRI, hysteroscopy, etc.
-
How findings guide treatment decisions
-
Limitations, pitfalls, and when further evaluation is needed
What Are Uterine Fibroids and Why Accurate Diagnosis Matters
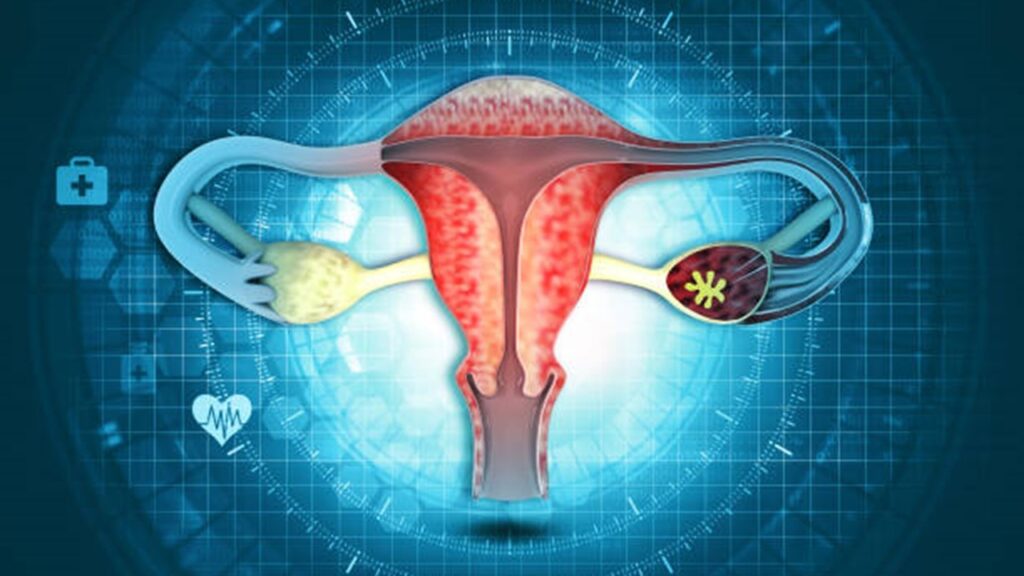
Uterine fibroids are noncancerous growths of the muscular wall of the uterus (myometrium). They vary by:
-
Location:
• Intramural (within the uterine wall)
• Submucosal (projecting into the uterine cavity)
• Subserosal (on the outside surface) -
Size & number: From tiny (millimeters) to very large, single or multiple.
-
Symptoms: Heavy or irregular bleeding, pelvic pain/pressure, urinary or bowel symptoms, infertility, or asymptomatic.
Accurate diagnosis is crucial because:
-
Treatment options depend heavily on location (e.g. submucosal fibroids may cause bleeding and fertility issues more than subserosal).
-
Size and number influence choices: medical vs surgical vs less invasive procedures.
-
Fibroid diagnosis also requires distinguishing them from other causes of uterine masses or bleeding (e.g. adenomyosis, polyps, malignancy).
Clinical Evaluation: History & Physical Exam
Before ordering imaging, doctors perform a thorough evaluation:
-
Medical / Gynecological History:
-
Menstrual history: length, regularity, flow amount, frequency, clots, bleeding between periods.
-
Symptoms of bulk effect: pelvic pressure, urinary frequency or retention, constipation.
-
Pain: cramping, back pain, dyspareunia (pain during intercourse).
-
Obstetric history: pregnancies, deliveries, fertility issues.
-
Risk factors: family history of fibroids, ethnicity (e.g. higher prevalence in African descent), obesity, early menarche.
-
-
Physical / Pelvic Examination:
-
Palpation: On pelvic or abdominal exam, enlarged, irregular uterus may be felt.
-
Size estimation: How large the uterus appears (e.g. compared to gestational age).
-
Whether there is tenderness, mobility limitations, or masses.
-
Often, fibroids are discovered incidentally in women who are being evaluated for other issues. Studies show transvaginal ultrasound picks up fibroids in many women even without symptoms.
Laboratory Tests
These are usually adjuncts, not definitive for diagnosing fibroids—but they help in evaluating symptoms and ruling out other causes.
-
Complete Blood Count (CBC): To assess for anemia, which may result from heavy bleeding.
-
Hormone / Thyroid Tests: To exclude thyroid disorders (hypothyroidism or hyperthyroidism) that may contribute to menstrual irregularities.
-
Pregnancy Test: To rule out pregnancy, molar pregnancy, or miscarriage—especially in women with bleeding.
-
Coagulation Profile: If there is suspicion of bleeding disorders.
-
Other labs depending on patient history: kidney/liver function if medications or co-morbidities are involved.
Imaging & Diagnostic Procedures
Imaging is essential in fibroid diagnosis. Several modalities exist; choosing the right ones depends on the clinical scenario, resources, and what information is needed.
Ultrasound (Transvaginal & Transabdominal)
Ultrasound is the most used initial diagnostic imaging tool. It is non-invasive, widely available, relatively inexpensive, and has good sensitivity.
-
Transvaginal ultrasound (TVUS) gives close-up images of the uterus and adnexa. It is more sensitive for smaller fibroids, submucosal fibroids, and uterine cavity distortions.
-
Transabdominal ultrasound (TAUS) may be more useful for large fibroids, or when TVUS is not feasible.
What ultrasound can show:
-
Size, number, and location (intramural, subserosal, submucosal) of fibroids.
-
Echogenicity (whether fibroid is hypoechoic, heterogeneous, calcified). Fibroids often appear as well-defined, solid, hypoechoic masses.
-
Relation to endometrium: is there distortion, displacement, or thinning or thickening?
Enhanced ultrasound techniques:
-
Saline infusion sonography (SIS) or hysterosonography: saline is infused into the uterine cavity to better delineate submucosal fibroids or uterine lining abnormalities.
Limitations:
-
May miss very small fibroids or those that are isoechoic with surrounding tissue. Subserosal fibroids or those outside the uterine contour may be harder to detect.
-
Operator dependency: quality depends on skill of sonographer and quality of equipment.
Magnetic Resonance Imaging (MRI)
MRI is used when:
-
Ultrasound findings are unclear.
-
Large or multiple fibroids, when precise mapping is needed before surgery or uterine artery embolization.
-
If adenomyosis is suspected (which can coexist or mimic fibroids).
What MRI offers:
-
High resolution in soft tissue contrast; better delineation of fibroid borders, internal characteristics (e.g. degenerative changes, necrosis, hemorrhage).
-
Accurate detection of submucosal vs intramural vs subserosal fibroids; assessment of size, volume, location relative to uterine and pelvic anatomy.
-
Helps in planning treatments like surgical removal or embolization.
Drawbacks:
-
More expensive, less accessible in some settings.
-
Longer exam time.
-
In rare cases, patients with implants, metal or claustrophobia may have difficulty.
Hysteroscopy
Hysteroscopy involves direct visualization of the uterine cavity by inserting a thin, lighted telescope (hysteroscope) through the cervix. Useful for:
-
Identifying submucosal fibroids that impact the uterine lining and bleeding or fertility.
-
Potentially removing small fibroids or polyps during the procedure.
-
Visualizing intracavitary lesions accurately.
It may be done in clinic or operating room; may require anesthesia depending on patient comfort.
Other Imaging or Diagnostic Procedures
-
Laparoscopy: To inspect the external surface of uterus, ovaries, tubes, and pelvic cavity. More invasive; used when there are other suspected pelvic pathologies.
-
Hysterosalpingography (HSG): An X-ray procedure with contrast to look at uterine cavity and fallopian tubes; used sometimes in infertility evaluation. Can incidentally identify some submucosal fibroids.
-
Computed Tomography (CT) Scan: Usually not first-line; fibroids can be seen, especially if large, but tissue contrast is poorer, and CT involves radiation. CT is more often used when other diagnoses are being considered.
Interpreting Findings: Key Elements Doctors Look For
When doctors review test/imaging results, they evaluate multiple features. These features help in distinguishing fibroids from other conditions and determining appropriate management.
| Feature | What to Assess | Why It Matters |
|---|---|---|
| Number and Size | How many fibroids, their diameters (or volume), growth rate if prior imaging exists. | Influences treatment type: may need surgery or embolization if large or many; small fibroids may be monitored. |
| Location | Intramural vs submucosal vs subserosal; whether protruding into cavity. | Submucosal fibroids often cause heavy bleeding or fertility issues; location can affect choice of removal method. |
| Effect on Uterine Cavity/ Endometrium | Degree of distortion, displacement, or compression. | Affects bleeding, fertility, and surgical accessibility. |
| Degeneration, Necrosis, Hemorrhage | Internal changes seen on MRI or ultrasound (dark or bright areas, heterogeneous textures). | May present with acute pain; may mimic other pathology; influences urgency or type of treatment. |
| Other Pelvic Structures | Uterine size, impact on bladder or bowel, presence of other masses (ovarian, etc.). | Helps to assess symptoms due to pressure; guides surgical planning. |
| Rule Out Malignancy / Other Conditions | Features such as rapid growth (especially after menopause), unusual imaging features, suspicion on MRI, biopsy where needed. | Uterine sarcoma is rare but serious; must be considered if features raise concern. |
How Diagnostic Findings Guide Treatment Decisions
After obtaining imaging and test results, doctors use them together with patient symptoms, fertility desires, and overall health to decide treatment. Some decision factors include:
-
Symptom Severity: Heavy bleeding, pain, pressure to bladder, fertility concerns. If symptoms are mild and patient prefers to avoid surgery, medical or minimally invasive options may be first choice.
-
Fibroid Characteristics: Small, few, submucosal fibroids may be removed hysteroscopically; large or multiple intramural/subserosal ones may require myomectomy or uterine artery embolization.
-
Fertility Goals: Women who wish for future pregnancy often prefer uterine-preserving treatments. Location of fibroids especially matters (submucosal removal can improve fertility outcomes for some).
-
Risk of Anemia or Complication: Heavy bleeding leading to anemia may push for more aggressive treatment.
-
Access and Resources: Availability of MRI, minimally invasive surgery, interventional radiology, cost considerations.
-
Age and Menopause Status: Fibroids often shrink after menopause; age impacts risk-benefit of surgery and long-term outcomes.
Limitations, Pitfalls, and When Further Evaluation Is Needed
Although diagnosis has many tools, there are some pitfalls:
-
Missed Fibroids on Imaging: Smaller ones, or fibroids that are isoechoic or in unusual locations may be overlooked.
-
Mis-classification: Mistaking adenomyosis or other uterine pathologies (polyps, endometrial hyperplasia) for fibroids and vice versa. MRI helps here.
-
Over-treatment Risks: Removing fibroids that are asymptomatic or without impact may expose patients to surgical risks unnecessarily.
-
Malignancy Considerations: Leiomyosarcoma is rare, but fast growth after menopause, atypical imaging features warrant suspicion. Pathology is often required for definitive diagnosis.
-
Cost, availability, patient discomfort: MRI is more expensive; hysteroscopy or laparoscopy involve more invasiveness or anesthesia; patient tolerance matters.
Diagnostic Workflow: Typical Process in a Clinic Setting
Here’s a hypothetical but realistic workflow that doctors at Big Apple Medical Care might follow to diagnose uterine fibroids:
-
Initial presentation: Patient presents with heavy menstrual bleeding, pelvic pain, or pressure symptoms.
-
History taking & physical exam: Obtain full menstrual, obstetric, medical history. Pelvic exam to assess uterine size and possible masses.
-
Laboratory tests: CBC, pregnancy test, possibly thyroid, coagulation if indicated.
-
First imaging: Transvaginal ultrasound (TVUS) ± transabdominal ultrasound (TAUS). If negative or ambiguous, consider saline infusion sonography.
-
If needed, advanced imaging: MRI when ultrasound is inconclusive or for planning surgery or interventional radiology (embolization).
-
Procedural evaluation: If submucosal fibroids suspected or endometrial cavity involved, hysteroscopy may be done. Sometimes laparoscopy if external pelvic pathology suspected.
-
Interpretation & planning: Combine imaging findings with patient goals. Create treatment plan (medical management, surgical, noninvasive, watchful waiting).
-
Follow-up: Monitor symptoms, repeat imaging if growth suspected, check for anemia, etc.
Case Studies / Examples
To illustrate how diagnostic findings lead to different paths, here are some case examples:
Case A: Symptomatic Submucosal Fibroid in Young Woman Desiring Fertility
-
Presentation: 30-year-old woman with heavy bleeding, irregular periods, difficulty conceiving.
-
Tests: TVUS shows a 3 cm fibroid within the uterine cavity (submucosal). SIS confirms protrusion; hysteroscopy visualizes it. MRI not necessary for basic size/location.
-
Decision: Proceed with hysteroscopic removal to relieve bleeding and improve fertility prospects.
Case B: Multiple Large Intramural Fibroids Causing Bulk Symptoms
-
Presentation: 45-year-old woman with pelvic pressure, urinary frequency, heavy periods. Uterus palpably enlarged.
-
Tests: Ultrasound shows multiple intramural fibroids; MRI ordered for mapping; CBC shows mild anemia.
-
Decision: Given symptoms and size, options might include myomectomy vs uterine artery embolization, possibly guided by imaging from MRI. Patient’s desire to preserve uterus dictates choice.
Case C: Incidental Fibroid in Asymptomatic Woman
-
Presentation: 38-year-old woman has imaging for another reason (e.g. pelvic pain unrelated) and ultrasound shows small fibroids (< 2 cm) intramural, no heavy bleeding, no fertility concerns.
-
Decision: Watchful waiting; periodic monitoring; perhaps medical therapy if bleeding develops.
Summary & Key Messages
-
Uterine fibroids are common benign uterine tumors; many are asymptomatic but others cause significant symptoms.
-
Diagnosis starts with history and physical exam, followed by laboratory tests when needed.
-
Ultrasound (transvaginal + transabdominal) is the initial imaging modality of choice, often sufficient. Saline infusion sonography enhances visualization for certain fibroids.
-
MRI is reserved for complex cases, preoperative planning, or unclear findings.
-
Hysteroscopy, laparoscopy, or hysterosalpingography are additional procedures used when needed, particularly for intracavitary lesions or infertility evaluation.
-
Interpretation of imaging must consider number, size, location, effect on endometrium, impact on adjacent organs, and patient goals (bleeding control, fertility).
-
Management decisions should balance benefits vs risks, taking patient preferences into account.
At Big Apple Medical Care, our diagnostic approach to fibroids aims to be thorough, minimally invasive, and aligned with each patient’s individual needs. If you suspect fibroids, or are experiencing symptoms such as heavy periods, pelvic pressure, or fertility challenges, we encourage you to schedule a consultation. Early diagnosis allows more options, less invasive treatments, and better outcomes.